Why did NPfIT fail?
The National Programme for IT (NPfIT) in the UK’s National Health Service (NHS) was one of the most ambitious and costly IT initiatives ever undertaken in the healthcare sector. However, it faced numerous challenges and was ultimately considered a failure. Here are the primary reasons for its failure:
1. Scale and Complexity: The NPfIT was an extraordinarily large and complex project. It aimed to revolutionise IT across the entire NHS in England, including the creation of electronic health records for every patient and a national broadband network for the NHS. The sheer size and complexity made it difficult to manage.
2. Top-Down Approach: The program was largely driven from the top down, without adequate consultation and engagement with the end-users, mainly the clinicians and NHS staff. This led to a mismatch between the system’s design and the users’ actual needs.
3. Lack of Flexibility: The NPfIT was criticised for its one-size-fits-all approach. Healthcare settings are diverse, and a rigid system failed to accommodate the varying needs of different hospitals and clinics.
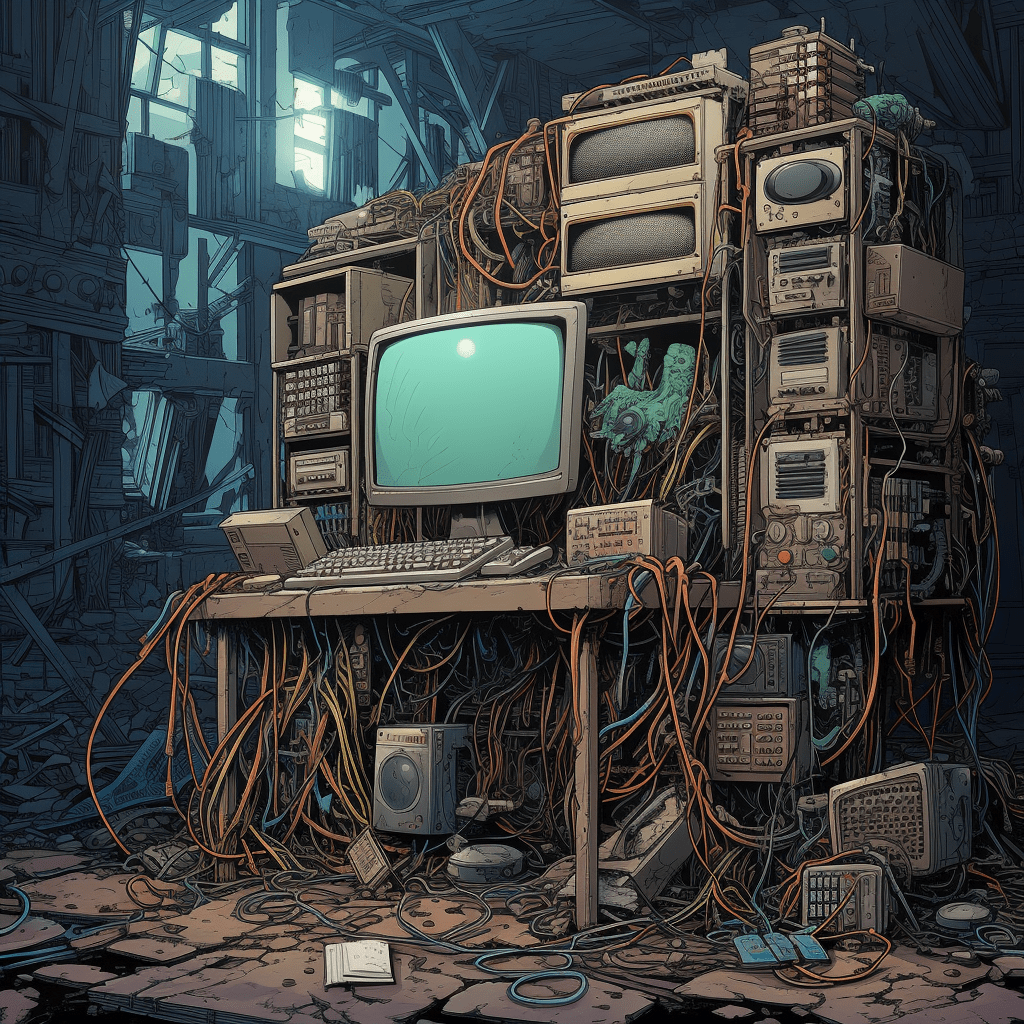
4. Technical Challenges: There were significant technical hurdles, including issues with software design and interoperability between different systems. Integrating new systems with existing legacy systems was also a major challenge.
5. Cost Overruns and Delays: The project faced significant cost overruns and delays. Originally estimated to cost around £6.2 billion, the costs reportedly ballooned to over £12 billion. Delays in delivery and deployment further eroded confidence in the project.
6. Vendor Issues: The project relied heavily on a few large IT vendors, some of which were unable to deliver as promised. This reliance on external contractors also led to issues with accountability and quality control.
7. Change in Political and NHS Leadership: The NPfIT also suffered from changes in political and NHS leadership, which affected the continuity, focus, and direction of the program.
8. Privacy Concerns: There were significant concerns regarding patient privacy and the security of electronic health records, which led to resistance from both healthcare professionals and patients.In summary, the failure of the NPfIT can be attributed to its over-ambitious scope, lack of user engagement, inflexibility, technical challenges, cost overruns, vendor issues, leadership changes, and privacy concerns. These factors combined to make the program untenable, leading to its eventual dismantling.
Avoid the NPfIT and US Medical Records project failures
download here
Strategies to avoid NPfIT-type failures
To avoid the pitfalls experienced by the NPfIT and ensure the success of a future large-scale IT program, especially in a complex and sensitive sector like healthcare, several key strategies should be implemented:
1. Stakeholder Engagement: Actively involve end-users, such as healthcare professionals, in the planning and implementation stages. Understanding their needs and workflows is crucial for designing a system that is user-friendly and adds real value to their work.
2. Incremental Approach: Rather than a big bang approach, adopt an incremental and agile methodology. This allows for regular feedback and adjustments, reducing the risk of large-scale failures and enabling more manageable project scopes.
3. Flexibility and Customisation: Recognise the diversity within the healthcare system and allow for a degree of customisation in different settings. A flexible system that can adapt to various environments is more likely to be successfully integrated.
4. Robust Project Management: Implement strong project management practices, including clear governance structures, regular progress reviews, risk management, and contingency planning.
5. Transparent and Realistic Budgeting: Set realistic budgets and timelines, and maintain transparency about costs and schedules. Regularly review and adjust budgets and plans as needed.
6. Vendor Management and Diversity: Diversify the range of vendors and avoid over-reliance on a few large suppliers. This can reduce risk and improve innovation. Rigorous selection criteria and performance monitoring should be employed.
7. Technical Excellence and Interoperability: Focus on high-quality software development practices. Ensure systems are interoperable, scalable, and compliant with standards to facilitate integration with existing and future systems.
8. Data Security and Privacy: Prioritise patient data security and privacy. Build robust security protocols and involve data protection experts. Transparent communication with patients about how their data will be used is essential.
9. Change Management: Recognise that introducing a new IT system is a major change. Provide adequate training and support to users, and manage the transition carefully to minimise disruption.
10. Continuous Learning and Adaptation: Establish mechanisms for continuous learning and improvement. Use data analytics and feedback to refine the system and adapt to changing needs.
11. Political and Leadership Support: Ensure consistent support from political and health system leaders. Leadership should be stable, committed, and aligned with the project’s goals.By addressing these areas, a future program can mitigate the risks associated with large-scale IT projects and increase the likelihood of a successful implementation.